Cervical Radiculopathy MRI
Cervical radiculopathy is a condition where one or more nerves in the neck (cervical spine) become compressed or irritated, resulting in symptoms such as pain, numbness, tingling, or weakness in the neck, shoulders, arms, or hands. To diagnose this condition, an MRI (Magnetic Resonance Imaging) is often employed, which helps doctors identify structural abnormalities that could be affecting the nerves in the cervical spine.
MRI
MRI is a medical imaging technique that uses strong magnetic fields and radio waves to generate detailed images of the internal structures of the body. Unlike X-rays or CT scans, which use radiation, MRI provides high-resolution images of soft tissues, such as muscles, nerves, and the brain. In the case of cervical radiculopathy, MRI is particularly useful in visualizing the cervical spine, which includes the vertebrae, intervertebral discs, spinal cord, and nerve roots.
Cervical Radiculopathy MRI
MRI of the cervical spine is a critical diagnostic tool for cervical radiculopathy, as it allows the physician to examine the structures of the neck region in great detail. The primary purpose of performing an MRI is to detect abnormalities that could be causing nerve compression. This includes issues like herniated discs, bone spurs, and narrowing of the spinal canal (spinal stenosis), all of which can put pressure on the nerve roots exiting the cervical spine.
The MRI creates detailed images of soft tissues, such as nerves, muscles, and discs, which may be involved in the compression of the nerve root. By examining these images, doctors can determine the exact location and cause of the nerve compression.
Cervical Radiculopathy MRI Images
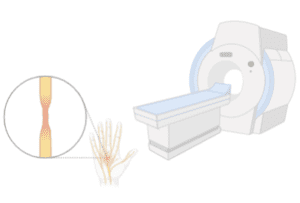
The MRI images of the cervical spine show a detailed view of the cervical vertebrae, intervertebral discs, and the nerve roots. These images can reveal several structural abnormalities, which may be contributing to the symptoms of cervical radiculopathy:
- Herniated Discs: A disc herniation occurs when the inner gel-like material of the disc bulges out, often pressing against a nearby nerve root. On MRI, this may appear as a bulging or ruptured disc that is out of its normal position, causing compression on the nerve root.
- Bone Spurs: These are bony growths that form on the vertebrae due to wear and tear, often causing nerve root compression. MRI can help identify these spurs and their location relative to the spinal nerve roots.
- Narrowing of the Spinal Foramen: The foramen is the opening where nerve roots exit the spine. When these openings become narrow, often due to disc degeneration or bone spurs, it can compress the nerves, causing symptoms of radiculopathy.
Cervical Radiculopathy MRI with or Without Contrast
MRI for cervical radiculopathy can be performed with or without the use of a contrast agent, which is a special dye that is injected into the bloodstream before the scan. This contrast agent helps provide more detailed images, particularly of soft tissues like nerve roots and tumors.
- Without Contrast: Most MRIs for cervical radiculopathy are performed without contrast. The high-resolution images generated are typically sufficient to detect structural issues, such as herniated discs or stenosis, which are common causes of nerve compression.
- With Contrast: Sometimes, contrast is used to enhance the MRI images, especially when the doctor needs more detailed views of soft tissues. This is particularly useful for detecting nerve inflammation, soft tissue tumors, or other issues not clearly visible without contrast.
Cervical Radiculopathy with Normal MRI
In some cases, an MRI may show no structural abnormalities, yet the patient still experiences symptoms of cervical radiculopathy. This is because MRI primarily identifies structural issues, but it may not always detect nerve inflammation, muscle spasms, or other functional problems that could cause radicular symptoms.
- Nerve Inflammation: Inflammation of the nerve roots might not be visible on a standard MRI but could still be causing significant symptoms.
- Muscle Spasms: Muscle spasms can compress nerves and cause pain or tingling, but these issues may not show up clearly on an MRI scan.
- Cervical Facet Joint Issues: Problems with the facet joints in the cervical spine, such as arthritis, might not be evident on a traditional MRI, yet they can still lead to symptoms of radiculopathy.
If an MRI shows no clear cause for the symptoms, other diagnostic methods, such as nerve conduction studies or electromyography (EMG), may be used to assess nerve function and identify the underlying cause of the radiculopathy.
Cervical Spine Radiculopathy MRI
A cervical spine MRI refers to the MRI of the entire cervical spine, which consists of the seven vertebrae (C1 to C7). A full scan of the cervical spine is necessary to evaluate the entire neck region for potential causes of radiculopathy. This includes detecting herniated discs, narrowing of the spinal canal (stenosis), bone spurs, or other abnormalities that may be pressing on the nerve roots. This comprehensive scan helps in providing a complete assessment of the cervical spine, allowing for a more accurate diagnosis and treatment plan. Since the neck is a complex structure, assessing the entire cervical region is crucial for understanding the full scope of the problem.
MRI plays a crucial role in diagnosing cervical radiculopathy by providing detailed images of the cervical spine, allowing doctors to identify the underlying causes of nerve compression, such as herniated discs, bone spurs, or spinal stenosis. Once the condition is diagnosed, treatment options like the Curapod device come into play.
Curapod uses electrical stimulation to manage the pain and discomfort caused by nerve compression, targeting the affected nerve roots to reduce inflammation, alleviate pain, and promote healing. Essentially, while MRI helps pinpoint the exact structural cause of the problem, Curapod is used as a treatment to address the symptoms and aid recovery, making them complementary tools in the management of cervical radiculopathy.


